Diabetes can lead to sensory neuropathy or loss of feeling in the feet and a minor foot problem of little significance to other people can be hazardous for people with diabetes. The importance of proper foot care in diabetes is widely recognised. It is recommended people with diabetes should be assessed by a podiatrist who will advise a daily care routine to reduce the risk of injuries and complications.
Diabetes affects the whole body, but the eyes, heart, kidneys and feet are at the greatest risk. People with diabetes are often admitted to hospital with foot problems more than for any other reason.
Diabetes may affect the feet in two ways. 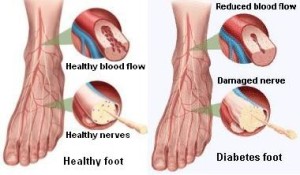
1. The nerves which enable you to feel pain, temperature extremes and give early warning of possible trauma, are damaged.
- Numbness
- A tingling, pins and needles sensation in the feet
- Burning pains in the legs and feet, usually more noticeable in bed at night.
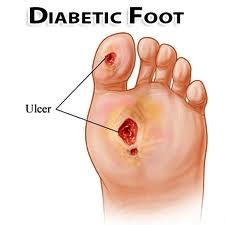
These symptoms can result in a loss of sensation in the feet which increases the risk of accidental damage because you can’t feel any pain. An injury to the feet can develop into an ulcer on the bottom of a foot which can penetrate to the bone. This could lead to infection of the bone (osteomyelitis) and a chronic infection in the bones and joints. If an infection isn’t treated at the earliest signs, this could result in ulceration (an infected open sore) and eventually amputation (removal of a toe, foot or limb).
Poor blood glucose control can cause a reduced supply of blood to the feet. This makes diabetic people more prone to infection following any injury that breaks the skin. Signs of poor blood supply include:
- Leg cramps after walking short distances or upstairs which is eased by resting. (Intermittent claudication)
- Pain in the feet, even at rest (often in the early hours of the morning)
- Feet feeling cold
- Feet looking a reddish-blue colour
- Cuts which take a long time to heal
Under these circumstances, even a minor foot problem of little significance to other people can be hazardous for people with diabetes. The importance of proper foot care in diabetes is widely recognised. It is recommended people with diabetes should be assessed by a podiatrist who will advise a common sense, daily care routine to reduce the risk of injuries and complications.
3. Role of podiatrists in diabetic foot management
As diabetes is a systemic disease affecting many different parts of the body, ideal case management requires a team approach. The podiatrist, as an integral part of the treatment team, has documented success in the prevention of amputations. The key to amputation prevention in diabetic patients is early recognition and regular foot screenings, at least annually, from a podiatrist.
In addition to these checkups, there are warning signs that you should be aware of so that they may be identified and called to the attention of podiatrists. They include:
- Skin colour changes
- Elevation in skin temperature
- Swelling of the foot or ankle
- Pain in the legs
- Open sores on the feet that are slow to heal
- Ingrown and fungal toenails
- Bleeding corns and calluses
- Dry cracks in the skin, especially around the heel
- Diabetic foot self-management education







 Mad Hat Media
Mad Hat Media